You would expect water in a hospital to be safe. But, far too often, water in hospitals and other healthcare facilities can put patients at risk of severe illness or death.
Since 2000, the United States has seen a 450% increase in cases of Legionella, the water-borne bacteria that causes Legionnaire’s disease, a serious form of pneumonia. Hospitals are susceptible to being Legionella breeding grounds due to aging facilities and inferior or improperly maintained water systems that provide the water for showers, faucets, ice machines, decorative fountains, cooling towers and more.
And because hospitals have many patients with underlying illnesses or weakened immune systems, the presence of Legionella or other waterborne pathogens in the water supply can be deadly.
Healthcare-associated infections (HAIs) even played a role in the Flint, Michigan, water crisis. While water supply-damaging lead pipes were the primary issue in Flint, a years-long investigation also revealed that a vast increase in cases of pneumonia there — including many that originated in a hospital before the lead pipe crisis — were tied to problems with the water system.
Even COVID-19 has been identified as a cause of several cases of Legionella in healthcare facilities. That’s because one of the primary causes of Legionella is water that becomes stagnant from settling in aging pipes for a long time. Facilities that shut down or had significantly reduced traffic in the early months of COVID-19 had water sitting idly in the piping system — and stagnant water can contribute to the development of the bacterium that causes Legionella and other waterborne, pathogen-related, HAIs.
The Centers for Disease Control and Prevention (CDC) estimates as many as 18,000 hospitalizations occur annually because of Legionella, with mortality rates ranging as high as 30%.
Besides unnecessary and preventable illnesses and deaths, Legionella and other waterborne HAIs wreak an enormous economic toll on healthcare systems and governments, too. A study conducted by Tufts University researchers revealed that the three most common waterborne pathogens directly cause hundreds of thousands of hospitalizations, requiring $9 billion in annual Medicare payments.
The CDC estimates that waterborne pathogens account for up to 30% of the annual $28.4 billion in total HAI costs, which is why the American Medical Association calls hospital water “perhaps the most overlooked, important, and controllable source of nosocomial infections.” A contributing factor is that many waterborne pathogens are antibiotic resistant, which makes the cost to treat a waterborne HAI more expensive. So, while plumbing systems generally account for less than 5% of healthcare construction costs, HIAs that can arise from flaws in the plumbing system can be very costly to remediate. Therefore municipalities that use prescriptive plumbing codes are well-served in helping to mitigate public health threats.
Eliminating waterborne HAIs will help healthcare organizations get the biggest return on investment, as these types of HAIs — more than any other — have the greatest negative impact on costs.
Taking the analysis even further, preventing HAIs, especially waterborne HAIs, provides an opportunity for healthcare facilities to generate revenue by backfilling patient beds. The result is that for each HAI eliminated by a hospital, an additional $1.5M in revenue can be generated. That opportunity can be realized by addressing plumbing system problems.
Waterborne HAIs are a monumental problem, but there’s plenty that hospital facilities managers and government officials — with a helping hand from the plumbing industry — can do to mitigate their impact and purge HAIs from the water supply. Doing so can save lives, protect reputations, lower costs, bolster revenues and, importantly, prevent deadly HAIs from returning in the future.
CAUSE AND EFFECT
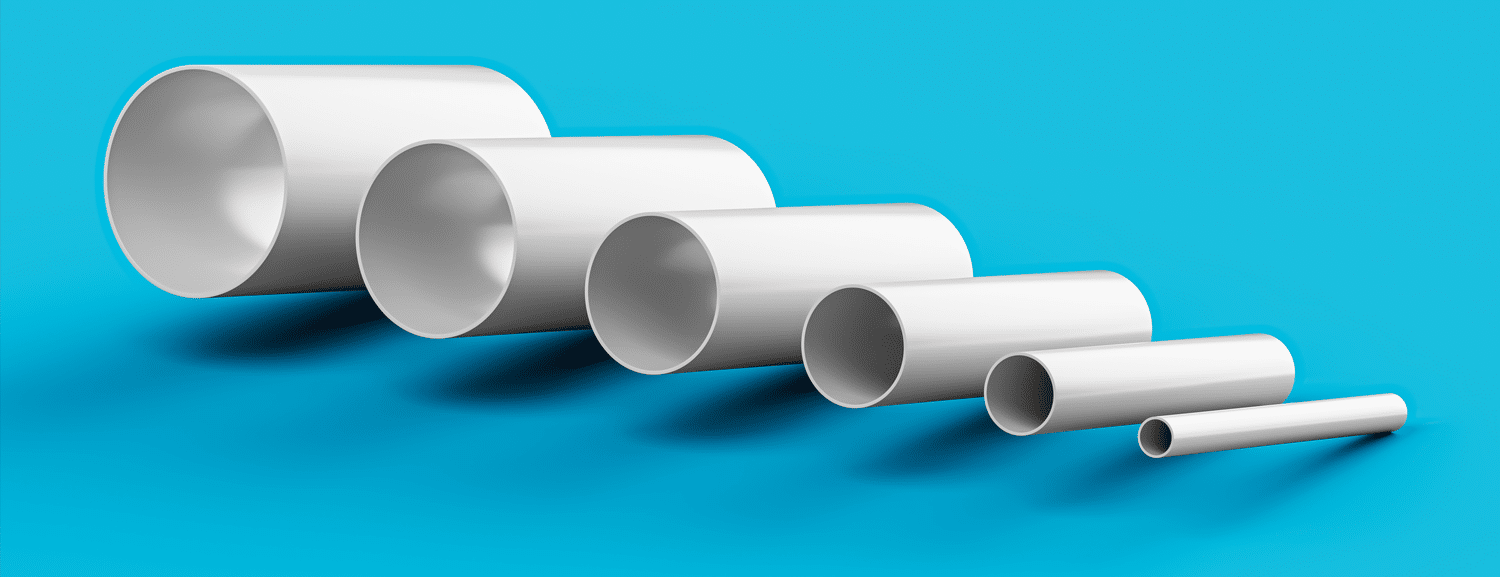
There are several primary causes of water-borne HAIs in hospitals. First, the size of the pipes used in hospital water systems can be a factor. Simply put, many pipes — especially in older systems — have a diameter that is larger than needed. That’s because in the last 30 years, after the passage of the Energy Policy Act of 1992 and heightened interest in sustainability initiatives, water flow rates and water volume use have decreased.
Unfortunately, water systems with oversized pipes can result in more instances of water stagnation, heightening the risk of waterborne pathogens in water pipes. That problem is further magnified in underutilized or temporarily shut down facilities, as pathogens growing in the stagnant water can lead to HAIs once the aged water begins flowing again.
Another contributing factor to HAIs is water temperature. Numerous research studies have confirmed that Legionella growth is enabled by lukewarm water temperatures, from about 77 to 108 degrees Fahrenheit. Thus, those water systems with insufficient circulation as well as lukewarm temperatures can be particularly susceptible to the growth of Legionella or other HAIs.
The good news is the plumbing industry — led by the non-profit International Association of Plumbing and Mechanical Officials (IAPMO), which develops and regularly updates industry codes that guide plumbing installation, maintenance and inspections — has revised its guidelines and is developing new procedures to help prevent or mitigate the pathogens that cause HAI outbreaks. And many of these guidelines are sure to be subsequently integrated into healthcare facilities’ Infection Control Plans (ICPs), which inform the engineering requirements for safely and effectively managing water systems.
For instance, the 2021 edition of IAPMO’s Uniform Plumbing Code (UPC®) addresses the Legionella issue in Appendix N; the UPC is the only model plumbing code that specifically addresses the subject. Additionally, IAPMO is currently working on a new guidance document titled “Construction Practices for Potable Water.” When finalized, the guidance’s research-driven insight will provide actionable and practical instructions to plumbing professionals during construction that will enhance how water systems work during the life of the building. Thoughtfully implementing preventative measures early in the building’s life cycle can result in “compound interest” of improved safety and cost savings.
IAPMO is working with the University of Cincinnati to expand the IAPMO Water Demand Calculator from residential buildings into commercial buildings, including healthcare. The Water Demand Calculator could reduce waterborne HAIs by right-sizing water systems, reducing water age and improving water quality.
A final version of the commercial Water Demand Calculator will take time to complete, but has the potential to become an additional tool to properly sizing water distribution systems in healthcare facilities.
Finally, IAPMO offers training to ASSE Legionella Standard 12080, Professional Qualifications Standard for Legionella Water Safety and Management Personnel, designated as an American National Standard by the American National Standards Institute (ANSI) for plumbing industry professionals to enhance their knowledge of microbiology, water quality and risk mitigation. IAPMO encourages builders and facilities managers who are planning, implementing or inspecting plumbing systems to consider seeking out water safety professionals who are certified to the ASSE Legionella Standard 12080, as it shows an acceptable level of competence in water safety and management specific to the Legionella issue.
Clearly, Legionella and HAIs are negatively impacting the health, wellness and economics of many communities, especially in healthcare settings. IAPMO continues to provide the most technically up-to-date solutions, via the UPC, developing techniques in water system design and maintenance, and offering world-class education. Through these activities, the risk of Legionella or other HAI outbreaks due to unsafe systems can be prevented — saving lives, reducing costs and improving outcomes for all stakeholders.

